COPAXONE iTracker® 2.0 Hack 1.4.2 + Redeem Codes
Injection Tracking Tool
Developer: Teva Pharmaceuticals USA, Inc.
Category: Medical
Price: Free
Version: 1.4.2
ID: com.tevapharm.itracker2
Screenshots


Description
COPAXONE (glatiramer acetate injection) iTracker® 2.0 has many features and resources which have been designed to help you track your past injections and plan for future ones:
• Injection Tracking – easily keep track of when and where you inject on your body
• Customizable Injection Settings – select your injection device, method, site, dosage, and schedule
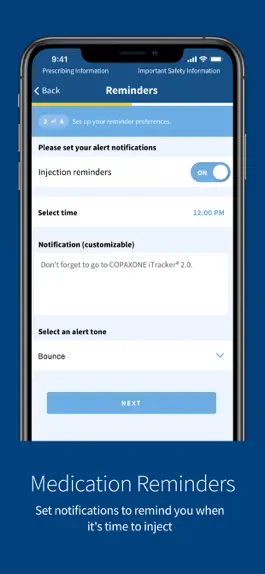
• Medication Reminders – set notifications to remind you when it’s time to take COPAXONE® (glatiramer acetate injection)
• Journal & Calendar – record injections, notes, and photos within your own personal journal. See past and future injections by using weekly or monthly calendar views
• Injection Reports – view, export, and share a history of your injections, notes, and photos
• Helpful Tips – get useful tips about injection best practices
Use
COPAXONE® is a prescription medicine that is used to treat relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
Important Safety Information
Do not use COPAXONE® if you are allergic to glatiramer acetate or mannitol.
Serious side effects may happen right after or within minutes after you inject COPAXONE® at any time during your course of treatment. Call your doctor right away if you have any of these immediate post-injection reaction symptoms including: redness to your cheeks or other parts of the body (flushing); chest pain; fast heart beat; anxiety; breathing problems or tightness in your throat; or swelling, rash, hives, or itching. If you have symptoms of an immediate post-injection reaction, do not give yourself more injections until a doctor tells you to.
You can have chest pain as part of an immediate post-injection reaction or by itself. This type of chest pain usually lasts a few minutes and can begin around 1 month after you start using COPAXONE®. Call your doctor right away if you have chest pain while using COPAXONE®.
Damage to the fatty tissue just under your skin’s surface (lipoatrophy) and, rarely, death of your skin tissue (necrosis) can happen when you use COPAXONE®.
Damage to the fatty tissue under your skin can cause a “dent” at the injection site that may not go away. You can reduce your chance of developing these problems by following your doctor’s instructions for how to use COPAXONE® and choosing a different injection area each time you use COPAXONE®.
Liver problems, including liver failure, can occur with COPAXONE®. Call your healthcare provider right away if you have symptoms, such as nausea, loss of appetite, tiredness, dark colored urine and pale stools, yellowing of your skin or the white part of your eye, bleeding more easily than normal, confusion, or sleepiness.
The most common side effects of COPAXONE® include redness, pain, swelling, itching, or a lump at the injection site; rash; shortness of breath; flushing; and chest pain.
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of COPAXONE®. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects.
You are encouraged to report side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please read the Patient Information in the full Prescribing Information at www.COPAXONE.com
• Injection Tracking – easily keep track of when and where you inject on your body
• Customizable Injection Settings – select your injection device, method, site, dosage, and schedule
• Medication Reminders – set notifications to remind you when it’s time to take COPAXONE® (glatiramer acetate injection)
• Journal & Calendar – record injections, notes, and photos within your own personal journal. See past and future injections by using weekly or monthly calendar views
• Injection Reports – view, export, and share a history of your injections, notes, and photos
• Helpful Tips – get useful tips about injection best practices
Use
COPAXONE® is a prescription medicine that is used to treat relapsing forms of multiple sclerosis (MS), to include clinically isolated syndrome, relapsing-remitting disease, and active secondary progressive disease, in adults.
Important Safety Information
Do not use COPAXONE® if you are allergic to glatiramer acetate or mannitol.
Serious side effects may happen right after or within minutes after you inject COPAXONE® at any time during your course of treatment. Call your doctor right away if you have any of these immediate post-injection reaction symptoms including: redness to your cheeks or other parts of the body (flushing); chest pain; fast heart beat; anxiety; breathing problems or tightness in your throat; or swelling, rash, hives, or itching. If you have symptoms of an immediate post-injection reaction, do not give yourself more injections until a doctor tells you to.
You can have chest pain as part of an immediate post-injection reaction or by itself. This type of chest pain usually lasts a few minutes and can begin around 1 month after you start using COPAXONE®. Call your doctor right away if you have chest pain while using COPAXONE®.
Damage to the fatty tissue just under your skin’s surface (lipoatrophy) and, rarely, death of your skin tissue (necrosis) can happen when you use COPAXONE®.
Damage to the fatty tissue under your skin can cause a “dent” at the injection site that may not go away. You can reduce your chance of developing these problems by following your doctor’s instructions for how to use COPAXONE® and choosing a different injection area each time you use COPAXONE®.
Liver problems, including liver failure, can occur with COPAXONE®. Call your healthcare provider right away if you have symptoms, such as nausea, loss of appetite, tiredness, dark colored urine and pale stools, yellowing of your skin or the white part of your eye, bleeding more easily than normal, confusion, or sleepiness.
The most common side effects of COPAXONE® include redness, pain, swelling, itching, or a lump at the injection site; rash; shortness of breath; flushing; and chest pain.
Tell your doctor if you have any side effect that bothers you or that does not go away. These are not all the possible side effects of COPAXONE®. For more information, ask your doctor or pharmacist. Call your doctor for medical advice about side effects.
You are encouraged to report side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please read the Patient Information in the full Prescribing Information at www.COPAXONE.com
Version history
1.4.2
2022-03-10
Bug fixes and performance improvements. This version now includes time stamps on all journal entries, in addition to an updated Privacy Policy and Terms of Use.
1.4.1
2022-03-03
Bug fixes and performance improvements. This version now includes time stamps on all journal entries, in addition to an updated Privacy Policy and Terms of Use.
1.3.1
2020-10-01
Bug fixes and performance improvements.
1.3
2020-08-31
Bug fixes and performance improvements.
1.1.1
2019-08-01
Bug fixes and performance improvements. This version now displays the last 14 injections on the home screen and improves load time.
1.1
2018-12-04
Previously recorded data has been removed to resolve technical issues related to Settings (device, reminders and schedule).
1.0
2018-10-19
Ways to hack COPAXONE iTracker® 2.0
- Redeem codes (Get the Redeem codes)
Download hacked APK
Download COPAXONE iTracker® 2.0 MOD APK
Request a Hack
Ratings
1.5 out of 5
209 Ratings
Reviews
MsAmyGS,
Was great but now it won’t open
I was using this app for about a month and it worked great. I really liked the reminders and the ability to track exactly which spot to give my next injection. However, since about 7/8/19, the app won’t open, just keeps spinning its wheels.
One suggestion that would make it better, once it gets back to opening properly, is to show where you gave the last injection without having to go back in the calendar to the previous dates... grey the spot out or something on the current injection spot options.
Hope it gets back to working soon.
One suggestion that would make it better, once it gets back to opening properly, is to show where you gave the last injection without having to go back in the calendar to the previous dates... grey the spot out or something on the current injection spot options.
Hope it gets back to working soon.
Retired pharmacist,
New app won’t open
I just downloaded the 2.0 app and tried to start it. I can’t get past the terms of use screens. I scroll to the bottom and push next but nothing happens. The text button doesn’t work.
2 days after above review: the app works now but I do not like it. I’ve used glatiramer injections since 2003, either as the brand or generic product and daily or 3 times a week. The transition to the generic product and new injection regimen was seamless using the first version. The first version is now disabled and I can’t access any of my injection history or notes. The new version has a different configuration on the injection site drawings. For example the abdominal drawing in the old version had 15 injection sites. The new version only has 11 sites so there is no correlation between the two apps. I made a Word table that is like the first version so I will use that rather than the 2.0 app. My own table was my reference when I changed to the new app as all my history from first version was lost. Without my table I would have had no record of where my last injection was given. This new app was a big disappointment and is not an example of good patient instructions.
2 days after above review: the app works now but I do not like it. I’ve used glatiramer injections since 2003, either as the brand or generic product and daily or 3 times a week. The transition to the generic product and new injection regimen was seamless using the first version. The first version is now disabled and I can’t access any of my injection history or notes. The new version has a different configuration on the injection site drawings. For example the abdominal drawing in the old version had 15 injection sites. The new version only has 11 sites so there is no correlation between the two apps. I made a Word table that is like the first version so I will use that rather than the 2.0 app. My own table was my reference when I changed to the new app as all my history from first version was lost. Without my table I would have had no record of where my last injection was given. This new app was a big disappointment and is not an example of good patient instructions.
RobJonSam,
Cost of medicine thousands of dollars
With the cost of this medication per month you would think they would hire a great app maker but noooo had to go from an ok app we all got used to to this junk , why is it so hard to make an app that simply lets you record and keep track of injections I mean so many more complicated apps out there that are free run way better than this app which cost us patients over thousands of dollars a month in meds . Are ya making an app just to shut us up with out thinking about functionality or ease of use ? Bad enough we have to struggle with a disease that ya refuse to find a cure to keep us drugged and paying for meds that don’t cure and only have a 33% probability, for the price of medication you’d think it was a cure, the least you can do is make a simple app for us . ZERO STARS
MS82',
Great App!
I’ve been using this app for about 5-6 yrs total. I love this app till 2 yrs ago the app started acting up (after 2 weeks of use the app kept freezing) and I deleted it, re-installed it again and again till I was finally fed up and deleted it for good. I’ve used other apps since then but other apps didn’t work as well and easy as the Copaxone ITracker 2. I decided to try download it again and after 2 months of use, NO PROBLEMS. I’m so so happy all the bugs are fixed. Well done Copaxone 👏🏽
Post1421,
I’ve used it for years.
I’ve used this app for years now. I have to say there are others out there, but I can’t seem to get them to work. This one at least seems to work for the most part, but today for some reason it didn’t work and I’ve now missed my shot, something I don’t like to do. I’ve been on Copaxon since 2013 and all my data was moved to this app, as I trusted it more than my book that I never filled out. I don’t even know when I started using this app it’s been so long. I really hope it’s fixed soon. I don’t like missing shots.
Thanks to whoever reads this bye 🖖🏼.
Thanks to whoever reads this bye 🖖🏼.
Brenaj48,
Not a good app!
This version of the app is not useful at all. First, I lost all data from the old app. So when I set up the new one, I had to guess where I last injected. Not sure why you would do this when we are told over and over again to rotate injection sites. And why would you REDUCE the number of injection sites?!? Makes no sense. I also don’t like the fact that it doesn’t indicate what your last injection sites were in a particular location. And the site has been down, so I had to guess this morning where to inject today. Did you even ask for input from people who actually use the medication and the app? It appears not based on reviews. I just started to use the app, but at this point, pretty sure I will find more not to like about.
Phinneaus,
I’d make one adjustment
I use this app regularly but I also make notes on a piece of paper because the app only saves the most recent location in any area that I have administered the shot. I would like it to show the past several locations in The same area of the body so I can better rotate sites. Maybe in varying shades of color as to tell which was the most recent?
Easy update for improvement: I really wish this app supported badges. I rely on those a lot because sometimes my notifications get buried on the lock screen. please allow those!
Easy update for improvement: I really wish this app supported badges. I rely on those a lot because sometimes my notifications get buried on the lock screen. please allow those!
MacMan000001,
One star to four stars
How do you go from being a one star app to being a four star one? You finally had the one feature that you lost in your old version: showing your previous injection spots for each injection site. Thanks to the latest update they now finally will show the last 14 injection spots. Without this feature, the only thing the app was doing was telling you which part of your body to inject but not the specifics for those locations. Thanks for FINALLY fixing this. Next up… Downloading your injection history as a back up.
Devo59,
A step in the wrong direction
If I could rate it Zero stars or a Negative number I would!
The previous version of iTracker had much more flexibility, planning & usable information. The current version removed
1) ability to adapt and change/update your injection schedule
2) the ability to view your injection schedule
3) the ability to easily update injection settings
4) reduced the amount of injection sites promoting injection in the same location
5) removed numbering system that allowed you to keep track of your injection schedule
6) doesn’t open up so even when it could help it doesn’t
In my view iTracker 2.0 would be better if it was replaced with a laminated version of the injection sites. So you could keep track with a dry-erase marker. You are better off memorizing your injection order & getting a layout of the injection sites and a dry erase marker.
I have been tracking my injections for 8 years and have never seen a worse option for keeping track. I have been a Project Engineer for years and this is not how to keep track of your injections.
Kindest regards,
Kevin P
The previous version of iTracker had much more flexibility, planning & usable information. The current version removed
1) ability to adapt and change/update your injection schedule
2) the ability to view your injection schedule
3) the ability to easily update injection settings
4) reduced the amount of injection sites promoting injection in the same location
5) removed numbering system that allowed you to keep track of your injection schedule
6) doesn’t open up so even when it could help it doesn’t
In my view iTracker 2.0 would be better if it was replaced with a laminated version of the injection sites. So you could keep track with a dry-erase marker. You are better off memorizing your injection order & getting a layout of the injection sites and a dry erase marker.
I have been tracking my injections for 8 years and have never seen a worse option for keeping track. I have been a Project Engineer for years and this is not how to keep track of your injections.
Kindest regards,
Kevin P
MarnaH,
Terrible new version
I really miss the old version where I could easily see the date that I last used a particular site. It had a much better visual of the sites, with more options of where to inject on each site. Particularly bad with this version, while it says you can change the order of injection sites, there is no way to do that that works. I do a daily injection and each day it says my next injection is in my stomach. I have to swipe through each screen, or look st the whole body, and try to remember is it time for my right arm or my left arm? It’s frustrating and stressful and a daily reminder that one of the difficult symptoms of MS is memory, not to mention the trying to minimize stress.